Healthcare systems run on data, but patient care depends on how well that data flows. Every admission, diagnosis, treatment plan, discharge summary, and insurance claim adds another layer of information that must be accurate, accessible, and secure. This growing complexity is exactly why organizations increasingly rely on healthcare software development services to build secure, scalable systems that support modern clinical workflows.
While off-the-shelf Electronic Health Record (EHR) platforms offer basic functionality, they often struggle to align with unique clinical workflows, departmental dependencies, and long-term growth goals. Custom EHR solutions solve this gap by giving providers full control over functionality, integrations, and data governance.
Many healthcare organizations seek EHR software development, but understanding how to build an EHR system goes beyond choosing the right technology stack. It requires a deep understanding of clinical processes, regulatory requirements, user behavior, and interoperability standards. When designed with purpose, an EHR system doesn’t just digitize records; it improves care coordination, reduces operational friction, and strengthens patient outcomes.
In this blog, we will break down how to build an EHR system step by step, covering the strategic, technical, and operational considerations needed to create a solution that improves care coordination, boosts efficiency, and supports better patient outcomes over time.
What Is EHR in Healthcare?
Electronic Health Records (EHRs) are digital versions of a patient’s complete medical history, designed to be securely collected, stored, and shared across healthcare ecosystems. Unlike paper-based records or siloed systems, EHRs enable real-time access to patient data for authorized stakeholders such as physicians, labs, pharmacies, specialists, care teams, and even patients themselves. This centralized access improves clinical coordination, strengthens accountability, and reduces the risk of errors that can lead to delays or medical malpractice when systems are poorly maintained.
From lab results and diagnoses to prescriptions, hospital stays, and follow-up care, EHRs consolidate critical health information into one unified platform. Modern EHR systems are built with a wide range of EHR software features, such as clinical documentation, interoperability, decision support, and secure data sharing, all aimed at improving care quality and operational efficiency.
Following EHR implementation steps correctly, EHRs help simplify workflows, reduce administrative burden, and empower healthcare professionals to deliver more accurate, patient-centered care.
Why is an EHR System Necessary?
Healthcare operations today are too complex to rely on fragmented systems and manual processes. An Electronic Health Record (EHR) system brings structure, speed, and intelligence into daily clinical and administrative workflows, helping healthcare organizations operate more efficiently while delivering safer, higher-quality care. With the right EHR software features, you can manage growing volumes of data without compromising accuracy, compliance, or patient experience.
Health Information Storage
EHR systems centralize critical clinical data management such as medical histories, lab results, medications, allergies, and immunization records. This structured storage allows healthcare professionals to retrieve and analyze information instantly, reducing delays and minimizing the risk of missing or outdated data.
Administrative Workflows
One of the biggest reasons EHRs are necessary is their ability to streamline operational tasks. Scheduling, billing, documentation, time management, and patient outreach are automated through core EHR software features, freeing staff from repetitive manual work and improving overall productivity.
Communication and Connectivity
EHR platforms enable secure, real-time communication between healthcare providers and patients. Built-in messaging tools support faster coordination, clearer information exchange, and improved continuity of care, all while maintaining strict data security standards.
Result Management and Interoperability
EHRs allow clinicians to share lab results, imaging reports, and clinical updates with colleagues across departments or external facilities. Interoperability ensures multiple EHR systems can exchange data seamlessly, supporting coordinated treatment and reducing duplication of efforts.
Decision Support
Advanced clinical decision support features help providers adhere to evidence-based practices. Automated alerts, reminders, and screening prompts enhance clinical judgment, support preventive care, and reduce the risk of chronic disease complications.
Order Management
EHR systems simplify the creation, storage, and tracking of medical orders, including tests and prescriptions. This eliminates redundancy, improves clarity, and accelerates order execution across various care settings.
Patient Support
Patient portals are essential EHR software features that empower individuals to access their medical records, monitor health data, review educational resources, and actively participate in their care journey.
Assessing Service Quality
With built-in analytics and reporting tools, EHRs help healthcare organizations gather patient feedback and measure service performance. These insights guide continuous improvement efforts, enabling clinics and hospitals to refine processes and elevate care quality over time.
Key Benefits of EHR Systems
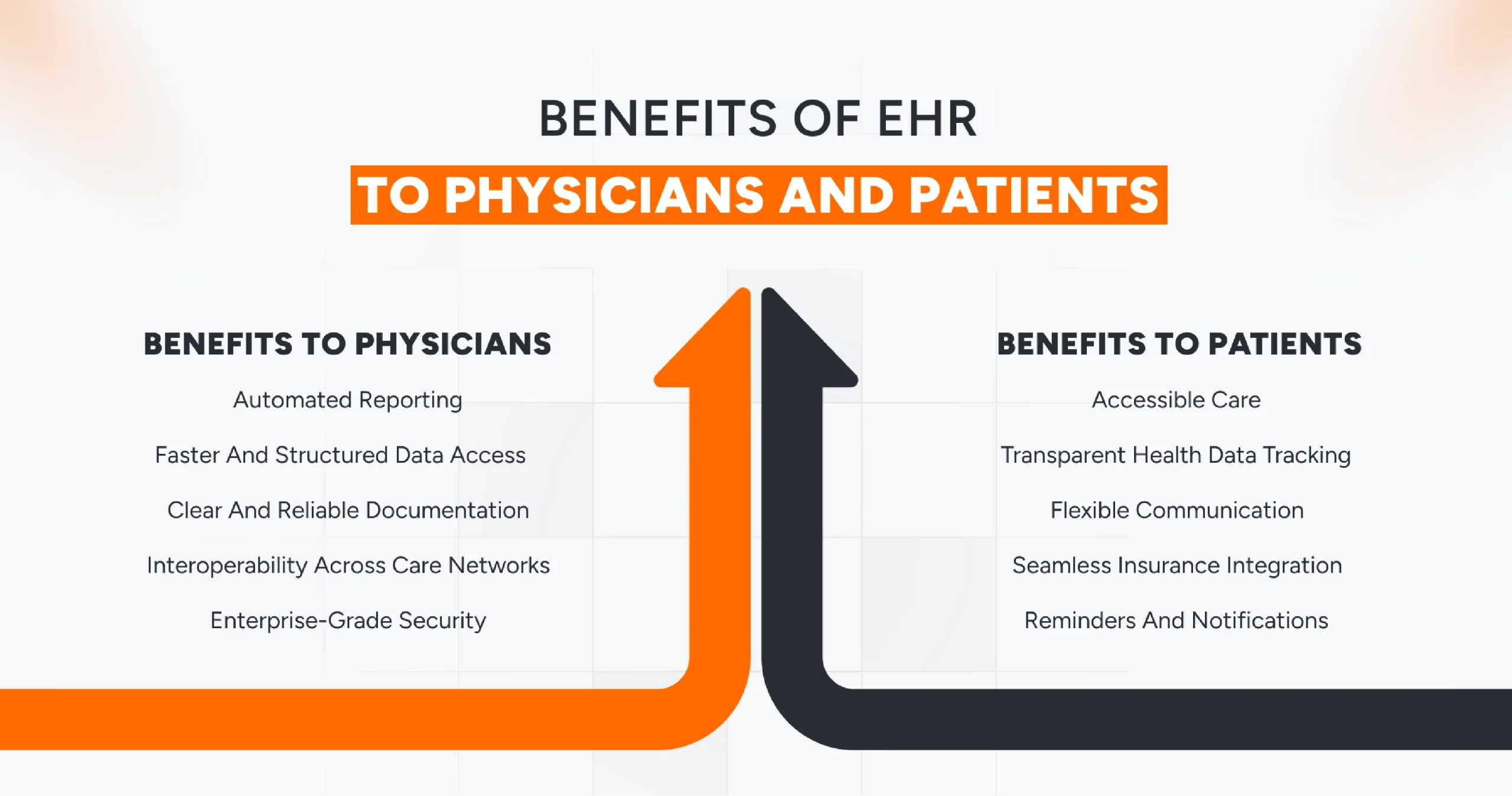
Electronic Health Record systems create a connected, intelligent healthcare environment where clinicians and patients stay aligned at every step of the care journey. When built with the right approach to EHR software development, these systems eliminate fragmented workflows, reduce repetitive data entry, and establish a single, reliable source of truth for medical information. The real value of EHRs lies in how their capabilities improve outcomes for both providers and patients through advanced EHR software features.
Benefits for Physicians
- Automated reporting: Regulatory compliance and operational oversight demand consistent reporting. Advanced AI-powered EHR systems simplify this with built-in reporting modules that automatically generate financial, clinical, medication, lab, and quality assessment reports, saving time and reducing manual errors.
- Faster and structured data access: EHR platforms organize complex clinical data into searchable dashboards, summaries, and alerts. Physicians gain instant access to critical patient information, helping them make faster, more informed decisions without digging through unstructured records.
- Clear and reliable documentation: Digital records eliminate the ambiguity of handwritten notes. EHRs maintain accurate, legible, and up-to-date patient information, highlighting essential details such as allergies, medications, and recent condition changes.
- Interoperability across care networks: One of the strongest EHR software features is seamless data exchange. EHR systems enable secure healthcare information sharing between clinics, labs, pharmacies, and specialists, reducing duplication and improving care coordination.
- Enterprise-grade security: Effective EHR software development prioritizes data protection. Role-based access control, encryption, audit logs, and compliance-driven security frameworks ensure sensitive health data remains protected against unauthorized access and cyber threats.
Benefits for Patients
- Always-on access to care: Cloud-based EHR systems provide continuous availability, allowing patients to connect with healthcare providers beyond clinic hours. This 24/7 access improves responsiveness and can be critical in urgent situations.
- Transparent health data tracking: Patient portals give individuals full visibility into their medical records. Test results, diagnoses, prescriptions, and care instructions are accessible in one place, encouraging informed and proactive health management.
- Flexible communication channels: EHRs support digital communication through secure messaging, emails, and appointment scheduling while still enabling in-person visits. This flexibility improves convenience without compromising care quality.
- Seamless insurance integration: Advanced EHR software features include insurance data capture and validation. Patients can link policies quickly, check coverage details, and streamline claims or reimbursement processes.
- Smart reminders and notifications: Automated alerts act like a personal healthcare assistant, notifying patients about upcoming appointments, medication refills, bills, follow-ups, and preventive checkups, helping them stay consistent with their care plans.
These benefits are best achieved through custom healthcare software development, where systems are designed around real clinical and operational requirements rather than generic templates.
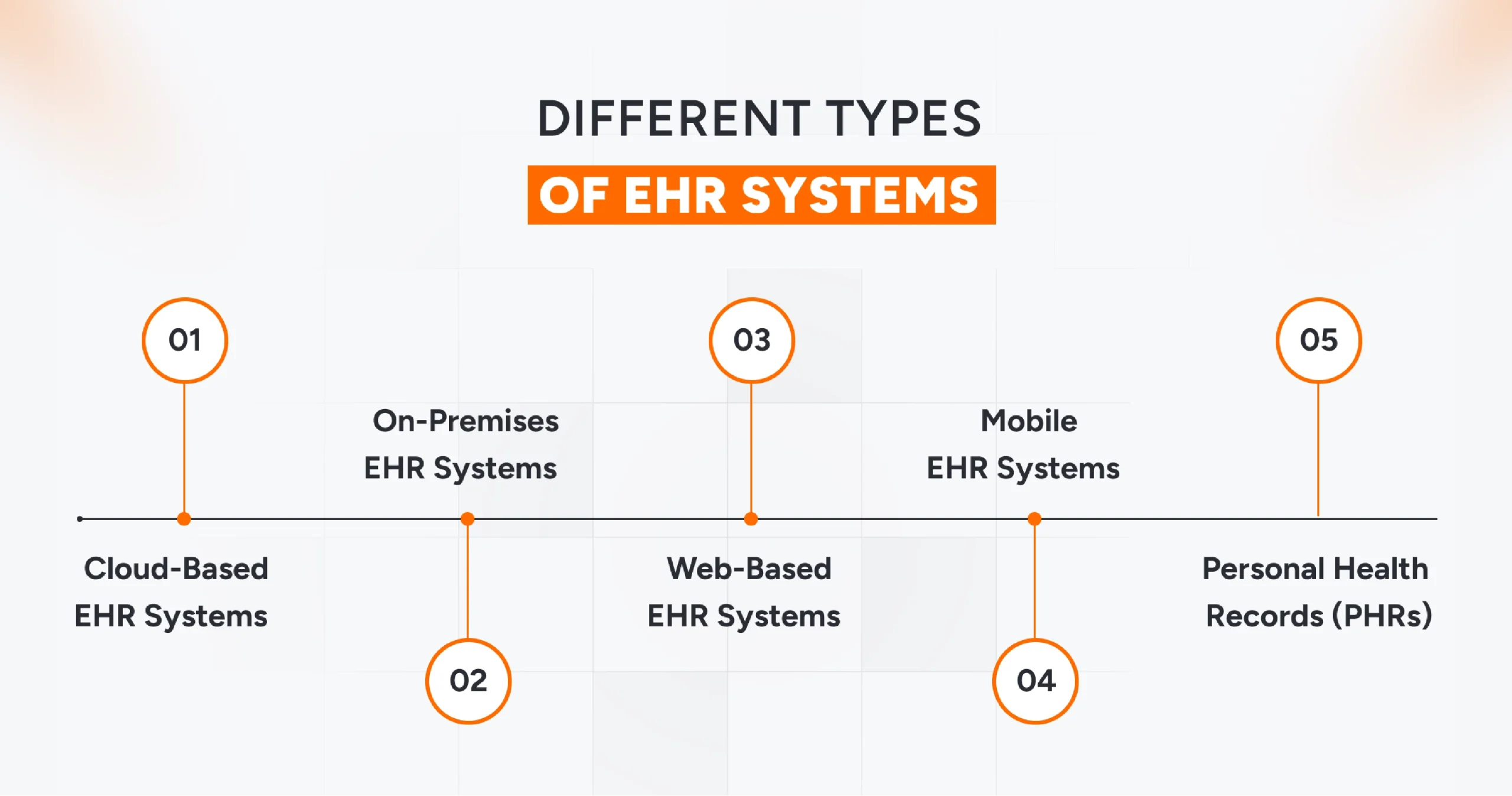
Different Types of EHR Systems
Not all Electronic Health Record systems are built the same. From a technical and operational perspective, EHR platforms come in multiple forms, each designed to support specific care models, access needs, and infrastructure requirements. Choosing the right type is a critical decision in EHR software development, as it directly impacts scalability, data access, security, and long-term usability.
Below are the most common types of EHR systems used across the healthcare industry today.
Cloud-based EHR Systems
Cloud EHRs are hosted on remote servers and accessed over the internet, making them highly scalable and cost-efficient. Healthcare professionals can retrieve patient data anytime, from anywhere, which is ideal for organizations with distributed teams or multiple locations. In EHR software development, cloud-based systems are often preferred for their faster deployment, automatic updates, and reduced infrastructure burden.
On-premises EHR Systems
On-premises EHRs are installed and maintained within a healthcare organization’s local infrastructure. This model offers greater control over data storage, security, and system customization. However, it also places full responsibility for maintenance, upgrades, and compliance on the organization, making it more resource-intensive from a development and operational standpoint.
Web-based EHR Systems
Web-based EHRs operate through standard web browsers, eliminating the need for complex local installations. They are especially useful for healthcare providers who require remote access or operate across multiple facilities. From an EHR software development perspective, these systems balance accessibility with centralized management.
Mobile EHR Systems
Mobile EHRs extend functionality to smartphones and tablets, allowing clinicians to access records, update notes, and review patient information on the move. These systems support faster decision-making at the point of care and are increasingly integrated into modern EHR development strategies.
Personal Health Records (PHRs)
PHRs are patient-centric systems that allow individuals to track their own health data, including appointments, medications, test results, and wellness metrics. While often connected to provider EHRs, PHRs focus on patient engagement and transparency, making them an important extension of comprehensive EHR software development initiatives.
Understanding these different EHR system types helps healthcare organizations align technology choices with clinical workflows, compliance needs, and future growth plans, ensuring the EHR solution supports both providers and patients effectively.
How to Build an EHR System: Detailed Step-by-Step Process
Building a custom EHR system is a strategic journey that blends clinical insight, regulatory readiness, and thoughtful EHR software development. A successful system evolves with its users, supports compliance, and delivers practical EHR software features without overwhelming clinicians.
Below is a structured breakdown of the essential EHR implementation steps to help you move from idea to impact.
Step 1: Define Clear Goals and Objectives
Before discussing features or technology, start with people. Engage doctors, nurses, administrative staff, and even patients to understand current pain points, workflow gaps, and unmet needs. These insights form the foundation of an EHR system that solves real problems instead of creating new ones.
Step 2: Plan Architecture and Compliance Early
Select an architecture, whether monolithic, microservices, or serverless, that aligns with your existing healthcare IT environment and future scalability plans. At the same time, map out compliance requirements and interoperability standards. Security planning should include encryption methods, role-based access, audit trails, and data governance policies from day one.
Step 3: Choose Practical, Scalable Technologies
Technology decisions should prioritize reliability and maintainability over trends. Whether it’s frontend frameworks or backend services, choose tools your development team understands and can scale confidently. Stability, performance, and long-term support matter far more than impressive tech stacks.
Step 4: Design for Speed and Simplicity
An EHR interface should feel intuitive within seconds. Physicians and staff operate under constant time pressure, so workflows must be clean, logical, and frictionless. Effective EHR software features focus on usability, such as quick chart updates, easy navigation, and minimal clicks for common tasks.
Step 5: Build an MVP First
Instead of launching a fully loaded system, begin with a focused MVP. Core modules such as patient profiles, clinical notes, appointments, e-prescriptions, and billing are enough to validate usability and performance. Once stable, expand functionality incrementally based on real user feedback.
Step 6: Make Security Non-Negotiable
EHR systems handle highly sensitive data, so implementing strong encryption, strict access controls, and continuous activity logging is crucial. Conduct regular vulnerability testing to ensure your system meets both regulatory and real-world security expectations.
Step 7: Test, Launch, and Support Thoroughly
Before deployment, test every aspect that includes functionality, usability, performance, and compliance. After launch, invest in user training through onboarding sessions, documentation, and ongoing support to drive confident adoption from day one.
Step 8: Iterate and Scale with Purpose
An EHR system should never remain static, it should monitor usage patterns, collect feedback, and refine workflows continuously. As organizational needs evolve, introduce new modules and enhancements that align with long-term care and operational goals.
Following these EHR implementation steps ensures your system is not only technically sound but clinically effective, secure, and built to grow with your healthcare organization.
Tech Stack and Team Required For EHR Software Development
Team Required For EHR Software Development
Building a reliable and compliant EHR system requires a carefully structured EHR software development team, where each role contributes to the platform’s stability, usability, and regulatory readiness. Key team members include:
- Project Manager: Oversees timelines, resources, and risk management while ensuring the EHR software development process stays aligned with healthcare standards and business goals.
- Business Analyst: Translates clinical workflows and regulatory requirements into clear functional specifications for the development team.
- UI/UX Designers: Design intuitive, accessible interfaces that simplify complex patient data and improve clinician adoption.
- Frontend & Backend Developers: Build secure, scalable application layers that power core EHR functionalities and data processing.
- Mobile App Developers: Enable seamless access to EHR systems across mobile devices for clinicians and patients.
- Quality Assurance (QA) Testers: Validate performance, security, interoperability, and compliance before deployment.
- DevOps Engineers: Manage cloud infrastructure, automate deployments, and ensure high availability of the EHR platform.
What Regulations to Consider When Building EHR Software?
As you progress through the EHR implementation steps, your system must be designed to protect sensitive patient data, support secure data exchange, and comply with region-specific legal requirements. From enforcing strong access controls and encryption to conducting regular security risk assessments and supporting standardized data exchange, compliance must be embedded into the foundation of your EHR system.
Below are the key regulations and standards to consider when building a compliant EHR platform:
HIPAA (Health Insurance Portability and Accountability Act)
HIPAA governs the protection of patient health information in the United States. It mandates strict controls over data access, storage, and transmission, along with clear breach notification protocols. Any EHR handling U.S. patient data must implement role-based access, audit trails, and strong security safeguards to remain compliant.
GDPR (General Data Protection Regulation)
GDPR applies to organizations operating in or serving users within the European Union. It places individuals in control of their personal data, requiring explicit consent, data transparency, and the right to access or erase information. EHR systems must be built to support these rights without compromising system integrity.
HITECH Act (Health Information Technology for Economic and Clinical Health)
The HITECH Act accelerated digital healthcare adoption in the U.S. while increasing accountability for data breaches. It strengthens HIPAA enforcement and requires healthcare systems to demonstrate meaningful use of EHRs through secure, auditable processes.
HL7 (Health Level Seven)
HL7 is a foundational interoperability standard that enables seamless data exchange between EHRs, labs, pharmacies, and other healthcare systems. Without HL7 compliance, your EHR risks becoming a silo rather than a connected healthcare solution.
FHIR (Fast Healthcare Interoperability Resources)
FHIR modernizes healthcare interoperability by enabling API-driven, real-time data exchange. Built for today’s applications, it allows EHR platforms to integrate easily with mobile apps, third-party tools, and future healthcare technologies.
By aligning regulatory requirements with technical architecture early in the EHR software development lifecycle, organizations can streamline implementation, reduce compliance risks, and build systems that are secure, interoperable, and future-ready.
Conclusion
EHR software development has become a necessity for healthcare organizations aiming to deliver connected, efficient, and patient-centric care. A well-built EHR system strengthens clinical workflows, improves data accuracy, supports compliance, and enables smarter decision-making at scale. With the right approach, EHR platforms can adapt to evolving care models while remaining secure and interoperable.
At AQe Digital, we leverage cutting-edge technologies, AI/ML capabilities, and advanced data analytics to build high-performance healthcare software with precision and quality at every stage. Our focus on scalable architecture and real-world usability ensures long-term value for healthcare providers and patients alike. If you’re planning to build or modernize an EHR system, feel free to contact us to discuss your requirements.
FAQs
The timeline depends on system complexity, required EHR software features, and compliance needs. A basic system may take a few months, while enterprise-grade platforms require phased development and iterative releases.
Core features include patient records management, clinical documentation, interoperability, role-based access, reporting, and secure data exchange. Advanced features may involve analytics, automation, and AI-driven insights.
Yes, custom EHR software development allows workflows, templates, and dashboards to be tailored for specialties like cardiology, pediatrics, or mental health, improving usability and clinical efficiency.
AI enhances EHR platforms by supporting predictive analytics, clinical decision support, automated documentation, and pattern recognition that help clinicians make faster, more accurate decisions.
Yes, when built correctly. Secure EHR software development includes encryption, access controls, audit logs, and compliance standards to protect sensitive health information in cloud environments.